Did you know that childhood trauma affects children differently than adults? What is childhood trauma exactly? It encompasses distressing experiences that overwhelm a child’s ability to cope, potentially affecting their development and well-being.
Children rank among the most vulnerable populations following traumatic events. Their reactions are significantly influenced by how you – their parents, caregivers, and teachers – respond. The childhood trauma definition extends beyond the event itself to include the child’s perception and response, which varies greatly based on age, personality, and support systems.
Every year, countless children experience traumatic events ranging from maltreatment to natural disasters. While some might exhibit clinging behaviors or tantrums, others may withdraw from family or avoid reminders of the event. Importantly, not all children exposed to trauma will develop post-traumatic stress disorder (PTSD), though many experience symptoms like nightmares or intense fear.
Your role as a parent or caregiver is crucial. Research shows that parenting stress is more common for those with PTSD, affecting the entire family dynamic. However, early intervention and stable supporting relationships can significantly mitigate the effects of childhood adversity and promote resilience.
This guide will help you understand, recognize, and respond to childhood trauma while supporting your child through their unique healing journey. Rather than viewing trauma as a permanent condition, you’ll discover how to foster recovery and growth in a trauma-informed environment.
Understanding the Impact of Trauma on Children
Understanding the Impact of Trauma on Children
Image Source: Kids Health
“The past can tick away inside us for decades like a silent time bomb, until it sets off a cellular message that lets us know the body does not forget the past.” — Donna Jackson Nakazawa, Science journalist and author of ‘Childhood Disrupted’
Trauma experienced during childhood leaves distinct marks on a child’s developing systems. Understanding these impacts helps you provide appropriate support for your child’s healing journey.
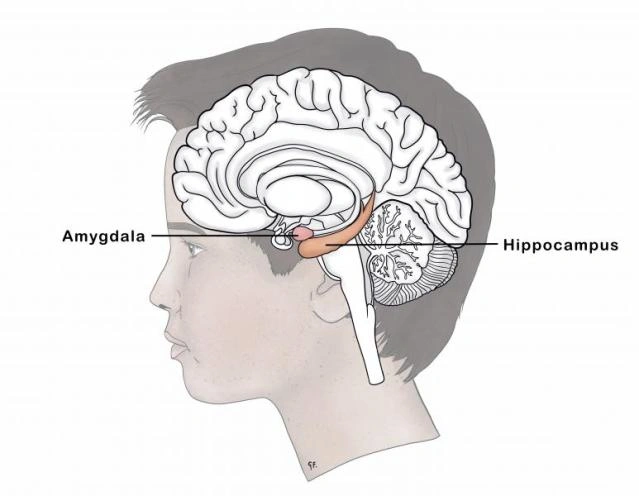
How trauma affects the brain and body
When a child faces traumatic stress, their body activates biological stress response systems that affect both brain development and physical health. The brain’s fear detection center—the amygdala—becomes activated, triggering a cascade of stress hormones throughout the body. This activation is the body’s natural way of responding to danger.
For children experiencing ongoing trauma, this stress response can become dysregulated. Research shows that childhood trauma can cause enlargement of the amygdala and shrinkage of the hippocampus, which is crucial for memory processing. Additionally, the prefrontal cortex, responsible for emotional regulation and decision-making, may show reduced thickness.
The hypothalamic-pituitary-adrenal axis (HPA)—the body’s central stress response system—undergoes significant changes in traumatized children. Scientists have observed that children with trauma histories often show alterations in cortisol levels, the primary stress hormone. Instead of following normal patterns, these levels may become either chronically elevated or abnormally low, depending on the nature and timing of the trauma.
Your child’s body responds to this dysregulation in various ways. Many children exhibit changes in heart rate, blood pressure, and immune system functioning. In fact, the body’s entire alarm system becomes recalibrated, making children more reactive to perceived threats even in safe environments.
Short-term vs. long-term effects
In the immediate aftermath of trauma, almost all children display some form of distress or behavioral change. These short-term reactions often include:
- Feelings of fear, sadness, or anger
- Sleep disruptions and nightmares
- Difficulty concentrating
- Physical complaints like headaches or stomachaches
- Regression in developmental milestones
- Heightened alertness to danger
Most children naturally recover from these initial reactions with proper support. Nevertheless, for some children, trauma exposure leads to more persistent challenges. Studies indicate that approximately 15% of girls and 6% of boys develop post-traumatic stress disorder following traumatic events.
Long-term impacts can be substantial if trauma isn’t addressed. Research from the Adverse Childhood Experiences (ACE) Study found that childhood trauma increases the risk of developing serious health conditions later in life, including heart disease, diabetes, and cancer. Furthermore, studies reveal that trauma can accelerate biological aging, with traumatized children showing faster cellular aging and early puberty compared to their peers.
Mental health consequences may persist into adulthood as well. Children with trauma histories face increased risk of developing depression, anxiety disorders, substance abuse problems, and difficulties with emotional regulation.
Why every child reacts differently
Despite experiencing similar traumatic events, children’s responses vary considerably based on multiple factors. First, developmental timing matters significantly. The brain has “sensitive periods” when specific regions are most vulnerable to trauma’s effects. Trauma occurring during these critical windows may have more profound impacts on particular brain functions.
The nature of the trauma also influences how a child responds. Research indicates that different types of traumatic experiences affect distinct brain regions. For instance, emotional abuse has been linked to delayed recovery of stress hormones following acute stress, whereas physical abuse is associated with faster stress reactivity.
Genetic factors contribute to differences in trauma responses as well. Studies show that certain genetic variations influence how the HPA axis responds to childhood trauma . Moreover, epigenetic changes—alterations in how genes express themselves without changing the genetic code—play a crucial role in determining long-term outcomes.
A child’s pre-existing support system forms another critical factor. Children with consistent, nurturing caregivers typically show greater resilience following trauma. In contrast, those lacking stable support may experience more severe and persistent effects.
Individual temperament and prior experiences also shape trauma responses. Some children naturally possess stronger self-regulation abilities or problem-solving skills that help them process traumatic experiences more effectively.
Understanding these varied responses helps you recognize that your child’s reaction to trauma is uniquely their own—neither “right” nor “wrong.” This awareness allows you to provide personalized support tailored to your child’s specific needs.
Recognizing Trauma in Everyday Behavior

Recognizing Trauma in Everyday Behavior
Image Source: CNA
Recognizing signs of childhood trauma requires careful observation of behavioral changes in your child. Children often lack the vocabulary or awareness to directly express their traumatic experiences, so their behaviors become the primary window into their emotional world.
Changes in mood or personality
Traumatic stress frequently manifests through noticeable shifts in a child’s emotional state. You might observe your previously cheerful child becoming withdrawn or irritable without apparent reason. Research indicates that approximately 60% of children experience emotional abuse during their lifetime, which can significantly alter their typical mood patterns.
Children with trauma histories commonly exhibit:
- Depression, anxiety, or unusual fears
- Sudden loss of self-confidence or self-esteem
- Emotional dysregulation (rapid mood swings)
- Excessive worry about safety
- Diminished interest in previously enjoyed activities
These mood changes aren’t simply “bad behavior” but rather adaptive responses to overwhelming experiences. For many children, depression symptoms might mediate associations between trauma and other behavioral issues. Consequently, you might notice your child becoming easily startled or constantly expecting something terrible to happen, even in safe environments.
Avoidance and withdrawal
Social withdrawal represents another common response to childhood trauma. Children may instinctively pull away from situations, people, or places that remind them of traumatic events. This withdrawal serves as a protective mechanism but can significantly impact their development.
Signs of avoidance include:
Frequently refusing to attend school or participate in social activities Isolating themselves from friends or family members Avoiding specific places, activities, or people that trigger memories Becoming unusually quiet or shut down in certain contexts
Studies show that socially withdrawn children are concurrently and predictively at risk for socio-emotional difficulties, peer problems, and school challenges. Yet it’s important to recognize that withdrawal isn’t merely shyness—it often reflects underlying difficulties of an emotional nature.
For some children, social withdrawal may appear as wariness around new people or reluctance to try new experiences. Approximately one in four students lives in a household affected by substance use (25.1%) or poor mental health (28.4%) , which can contribute to these avoidant behaviors as they attempt to navigate unpredictable environments.
Aggression or risk-taking
Perhaps surprisingly, childhood trauma can lead to seemingly opposite behavioral patterns—some children become more aggressive or engage in risky behaviors. This represents another adaptation to trauma, as children attempt to regain control or cope with overwhelming emotions.
Aggression might present as:
- Increased fighting, bullying, or hostility toward peers
- Unexpected angry outbursts or tantrums
- Physical aggression toward others or property
- Self-destructive behaviors
Research shows that youth who experienced four or more adverse childhood experiences (ACEs) had significantly higher prevalence of violence perpetration in the form of bullying, physical fighting, dating violence, and weapon carrying. Importantly, trauma exposure is a consistent correlate of intimate partner and parent-to-child aggression perpetration.
Risk-taking behaviors are equally concerning. Studies demonstrate strong patterns of clustering between smoking, binge drinking, illicit drug use, violence, and sexual behaviors in trauma-exposed youth. The strongest associations were observed between experiencing four or more ACEs and attempted suicide, seriously considering suicide, and current prescription opioid misuse.
Understanding these behavioral manifestations of childhood trauma enables you to respond with compassion rather than punishment. Remember that these behaviors, although challenging, represent your child’s attempt to cope with overwhelming experiences and feelings they may not yet understand or be able to express.
How to Talk to Children About Trauma
Communicating effectively about trauma requires sensitivity, honesty, and patience. According to child and adolescent psychiatrist Victor Carrion, honest, age-appropriate communication with children is one of the most important elements of helping youngsters handle traumatic events . Talking openly creates a foundation for healing and helps children make sense of their experiences.
Age-appropriate communication
Children process information differently at various developmental stages, requiring tailored approaches to discussing traumatic events. Primarily, start by asking what they’ve already heard. Most children will have heard something, regardless of their age. This creates an opening to correct misconceptions and provide accurate information.
For young children (age 5 and younger):
- Use simple, concrete language
- Avoid euphemisms that cause confusion
- Draw simple pictures to explain concepts
- Keep conversations brief
- Focus on safety and comfort
School-age children benefit from more detailed but still straightforward explanations. Use real words rather than euphemisms. For instance, say “Grandma has died, she is not coming back” instead of vague phrases like “She went to a better place”.
Teenagers and older children typically seek deeper understanding and may ask more questions about the “why” behind traumatic events. They can handle more nuanced discussions but still need emotional support throughout conversations.
Answering difficult questions
Children often ask challenging questions after trauma that can catch you off-guard. First thing to remember is to invite conversation in an open-ended way. When a child gives brief answers, follow up with “Okay, tell me more about that” to encourage elaboration.
When facing questions you don’t know how to answer, it’s perfectly acceptable to say: “I don’t know the answer to that and I’m not sure anyone does. I do know, nonetheless, that many thoughtful people throughout the world are working hard to understand this issue”.
Avoid leading questions that insert your own thoughts and feelings into the conversation. Questions like “That was a really bad car crash. You must really be hurting” can inadvertently influence how children process their experiences. Instead, ask open-ended questions such as:
- “How do you feel when you think about what happened?”
- “How often do you think about the event?”
- “What questions do you have about what happened?”
Reassuring safety and support
After a trauma, children need your support and comfort more than ever. Reassurance is the key to helping children through traumatic times. Even before starting any conversation, ensure the child is physically safe and fully aware they are out of harm’s way.
Physical comfort plays a crucial role in establishing security. All children, from toddlers to teens, benefit from extra cuddling, hugs, or reassuring pats on the back. These physical connections provide a feeling of security that’s essential after frightening events.
Be consistent in your messaging about safety. Remind children that:
- They are protected and safe now
- You will do everything possible to keep them safe
- People in the community are working to prevent similar events
- It’s okay to have all kinds of feelings about what happened
Establish soothing routines that provide structure and predictability. Take a few minutes at bedtime to read a story, snuggle together, or sing to young children. For older children, create a routine of giving a good night hug along with a few minutes to talk.
When discussing community tragedies, point out the helpers – police officers, doctors, and ordinary citizens whose acts restore faith in humanity. This helps children understand that even in difficult times, good people are working to keep everyone safe.
Essentially, your goal is to create an environment where children feel comfortable expressing their feelings without fear of judgment. Let them know it’s okay to be fearful, angry, or sad. By being a supportive listener and providing consistent reassurance, you help your child process trauma in healthy ways that foster resilience and recovery.
Supporting Your Child Through the Healing Process
The healing journey after childhood trauma begins with your consistent presence and support. Families experience trauma differently based on factors like a child’s age and cultural background. Primarily, your role as a caregiver is to create a healing environment where your child feels safe enough to process their experiences.
Being present and consistent
Children who have experienced trauma need comfort and stability more than ever. Spend quality time with your child doing activities that are soothing, relaxing, or fun – cooking together, taking walks, playing, reading, or singing. These seemingly small activities matter tremendously in trauma recovery.
Maintain a calm demeanor even when feeling overwhelmed yourself. Children exposed to trauma often experience lasting effects on their nervous system, leaving them in a near-constant state of sensory overload. Speak softly, use neutral tones, and avoid sudden movements. Whenever possible, let your child know what will happen beforehand to build predictability.
Physical comfort plays a crucial role in healing. Use hugs, smiles, and caring actions to show your love. Even teenagers benefit from appropriate physical reassurance through high-fives or brief hugs when welcomed.
Helping them express emotions
Many children who have experienced trauma find it challenging to understand their own feelings as well as the emotions of others. Fortunately, you can help by:
- Identifying feelings using emotion cards or feeling faces
- Connecting emotions to thoughts and behaviors through books or educational shows
- Modeling emotional regulation (“I’m feeling overwhelmed so I’m going to take deep breaths”)
- Creating safe spaces where all feelings are acceptable
Validate your child’s emotional experiences without judgment. Rather than saying “Don’t be scared,” confirm what you’re hearing: “Yes, I can see that you’re worried”. This validation teaches children that their emotions are normal and acceptable.
In addition, play offers children a natural way to process emotions and build resilience. Through pretend play, children can practice overcoming challenges in a safe, imaginative environment.
Balancing structure and flexibility
After trauma, children benefit greatly from the security of routines while also needing flexibility as they heal. Try to maintain regular daily schedules for meals, bedtime, and activities. These predictable patterns help children know what to expect, creating a sense of safety.
Meanwhile, temporarily reduce expectations about performance at school or home. Excuse traumatized children from chores for a day or two. After that initial period, reintroduce age-appropriate tasks that help them feel useful and connected to family life.
Gradually encourage children to resume normal activities while being patient with their progress. One parent described their approach: “Just trying to be normal and not baby him too much, to sort of encourage him to do things a bit more on his own but not wanting to push it too much… it’s still quite soon after”.
Above all, remember that recovery isn’t linear. Children often need repeated practice with vagus nerve balancing exercises that help regulate their nervous system. Simple techniques like shaking out tension, deep breathing, or light physical activity can help reset their stress response and support healing.
By combining consistent presence, emotional support, and balanced structure, you create the foundation your child needs to process trauma and build resilience for the future.
Creating a Trauma-Informed Home Environment

Balancing structure and flexibility
Image Source: Starr Commonwealth
“When a flower doesn’t bloom, you fix the environment in which it grows, not the flower.” — Alexander Den Heijer, Inspirational speaker and author
Your home environment plays a crucial role in your child’s recovery from trauma. Creating trauma-informed spaces requires thoughtful attention to physical surroundings, daily routines, and opportunities for empowerment. Indeed, the right environment can significantly reduce stress and support healing.
Reducing triggers and stressors
Children who have experienced trauma often become highly sensitive to certain stimuli that remind them of traumatic events. Initially, identify potential triggers by observing your child’s reactions to different situations, sounds, or visual elements. Pay attention to when they become agitated, withdrawn, or show other signs of distress.
To create a physically secure space:
- Ensure proper lighting (avoid harsh or extremely dim lighting)
- Maintain clear pathways throughout your home
- Reduce unnecessary noise and chaos
- Use soft textures like plush rugs or comfortable furniture
Manage your child’s exposure to potentially triggering media content, particularly news reports about traumatic events. Studies show that repeated exposure to such content can retraumatize children and increase anxiety. Therefore, limit screen time showing disturbing images or stories that might remind them of their experiences.
Using calming routines and rituals
Consistent routines provide a sense of predictability that helps traumatized children feel secure. Regular schedules for meals, homework, play, and bedtime create stability and reduce anxiety about what comes next. As one expert notes, “Regular routines provide a sense of stability and predictability. This can be as simple as consistent bedtimes, mealtimes, and daily activities”.
Incorporate calming activities into daily life:
- Warm baths with soothing scents
- Quiet reading time before bed
- Deep breathing exercises
- Gentle physical activities like walking outside
Sensory tools can be especially effective for younger children. Consider weighted blankets, fidget toys, or listening to calming music through headphones. These sensory inputs help calm lower brain systems that become dysregulated after traum .
Encouraging autonomy and choice
Trauma often leaves children feeling powerless. As a result, giving appropriate choices helps restore their sense of control. “Trauma can make a child feel powerless. Trauma-informed parenting emphasizes giving the child choices whenever possible, helping them regain a sense of control”.
Offer age-appropriate options throughout the day:
- “Would you like to wear the red or blue shirt today?”
- “Should we read a story or play a game this evening?”
- “Would you prefer having apples or oranges with lunch?”
Ultimately, involve your child in creating their own safe spaces at home. This might be a comfortable reading nook, a special corner with favorite toys, or a calming area where they can go when feeling overwhelmed. Such personalized spaces can be empowering and therapeutic, giving them ownership over their environment.
Remember that creating a trauma-informed home is an ongoing process that evolves as your child heals. By consistently providing safety, predictability, and appropriate autonomy, you help rebuild their sense of security in the world.
Working with Schools and Community Resources
Schools serve as critical support systems for children who have experienced trauma. Connecting your child’s home healing environment with educational settings creates a consistent approach that significantly improves recovery outcomes.
Collaborating with teachers and counselors
Building strong partnerships with your child’s educators begins with open communication. Schedule a private meeting with teachers to share appropriate information about your child’s experiences and current needs. Schools can provide comfort and stability, playing a vital role in maintaining normal routines after a crisis.
Fortunately, transparent communication works both ways. Request regular updates about your child’s classroom behavior and academic performance. As one trauma expert notes, “It is well established that parents and caregivers have tremendous influence on their children’s success in school”.
Remember that sharing power is essential in these partnerships. Specifically, approach teachers as equals in supporting your child, recognizing that each of you brings unique insights to the collaboration.
Accessing local mental health services
Mental health support is often a crucial element in trauma recovery. Generally, school counselors can connect you with local resources tailored to your child’s needs. Professional help is one of the most important steps a parent can take for a child with trauma exposure.
When seeking services, look for:
- Trauma-specific assessments and interventions
- Family-based therapy options
- Providers with childhood trauma specialization
Organizations like the National Child Traumatic Stress Network offer resources on various aspects of childhood trauma. Visit Support a Child’s Light (https://www.childslight.com/support-us/) to find additional trauma recovery programs and contribute to creating healing environments for affected children.
Advocating for trauma-informed practices
Undoubtedly, trauma-informed schools provide better support for children with trauma histories. These environments recognize trauma’s widespread impact and respond by integrating this knowledge into policies and procedures.
Advocate for your child by asking whether the school:
- Provides trauma-informed training for staff
- Implements positive behavioral supports
- Creates physically and emotionally safe spaces
Keep in mind that effective trauma-informed approaches require school-wide commitment. Primarily, this means involving school leadership as key members in developing systems that support students experiencing trauma.
By connecting home recovery efforts with school and community resources, you create a comprehensive support network that strengthens your child’s healing journey.
Understanding Treatment Options and What to Expect
Seeking professional help marks a critical step in addressing childhood trauma. Understanding what to expect throughout this process helps you navigate treatment options effectively and prepare your child accordingly.
Initial assessments and diagnosis
Professional evaluations typically begin with comprehensive screening measures like the Child Trauma Screen (CTS), which identifies trauma exposure and PTSD symptoms in children ages 6-17. These assessments gather information through parent interviews, caregiver questionnaires, and observations of parent-child interactions.
During initial evaluations, clinicians will assess:
- Specific details of traumatic experiences
- Changes in your child’s behavior
- Quality of primary attachment relationships
- Developmental delays that might require additional services
A thorough assessment creates the foundation for appropriate treatment planning. For children scoring 6 or greater on standardized measures, referrals for trauma-focused treatment are typically recommended.
Therapy types and goals
Several evidence-based treatments have proven effective for childhood trauma. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) stands among the most common, typically lasting 12-15 sessions. This structured approach helps children process traumatic memories while developing coping strategies.
Other effective therapies include Eye Movement Desensitization and Reprocessing (EMDR), which uses repetitive eye movements to reprocess frightening memories, and Dialectical Behavior Therapy for Children (DBT-C), which helps children regulate intense emotions.
Throughout treatment, therapy goals generally focus on symptom reduction, emotional regulation, and skill development. Your child’s therapist will likely monitor progress continuously, adjusting approaches as needed.
Involving the whole family in care
Family engagement significantly increases positive outcomes for trauma-affected children. Evidence-based practices frequently involve both the child and primary caregivers, as engaged parents aid the treatment process by ensuring attendance and reinforcing skills at home.
Organizations like Support A Child’s Light provide resources for families navigating trauma recovery together. Primarily, your participation helps your child feel supported throughout their healing journey.
Remember that seeking help represents strength, not weakness. With appropriate treatment and family involvement, children can develop resilience and heal from even significant trauma experiences.
Helping Your Child Build Resilience Over Time

Helping Your Child Build Resilience Over Time
Building resilience represents a crucial foundation for recovery from childhood trauma. As time passes, your consistent support combined with structured approaches helps children develop the inner strength to overcome adversity and thrive despite difficult experiences.
Celebrating small wins
Recognizing even minor progress powerfully impacts a child’s healing journey. Throughout recovery, acknowledge achievements like a full night’s sleep without nightmares, successfully managing emotions during stress, or engaging in new self-care activities. Many trauma survivors struggle to celebrate successes due to feelings of inadequacy or minimization of their achievements.
Create simple ways to mark progress:
- Keep a journal documenting positive moments
- Create visual representations like charts or pictures
- Share breakthroughs with trusted supporters
Celebrating small victories gives children a dopamine boost, changing brain chemistry and making them “feel good” naturally. Furthermore, these acknowledgments foster a supportive environment where children feel seen, heard, and valued for their strength.
Teaching problem-solving and self-regulation
Children with trauma histories benefit immensely from developing concrete skills to manage challenges. Given these points, introduce problem-solving by helping them:
- Define the problem clearly
- Brainstorm possible solutions
- Evaluate options
- Try the most promising approach
Self-regulation techniques like breathing exercises, writing activities, and identifying triggers help children manage distressing physical and emotional reactions . Certainly, providing “islands of competence” where children experience success combats the poor self-concept often associated with trauma.
Staying hopeful and connected
Hope serves as a powerful tool for resolving trauma, depression, and anxiety. Encourage your child to focus on positive qualities by asking what strengths they possess or what growth they’ve experienced through healing . In brief, maintaining these strengths-based conversations counters feelings of hopelessness.
Social connections prove equally vital—encourage activities and play with others to provide distraction and normalcy . Upon establishing safety, engage in family discussions about difficult experiences, allowing everyone to express emotions openly. Ultimately, the strongest protective factor linked with resilience to childhood trauma is the reliable presence of sensitive, nurturing adults in a child’s life .
Conclusion
Understanding childhood trauma requires patience, knowledge, and compassion. Throughout this guide, you’ve learned that trauma significantly impacts developing brains and bodies, yet children possess remarkable capacity for healing when provided appropriate support. Your role as a parent or caregiver remains the single most powerful factor in your child’s recovery journey.
Above all, remember that healing from childhood trauma happens gradually through consistent, trauma-informed approaches. Creating safe environments, maintaining predictable routines, and responding sensitively to behavioral changes allows your child to rebuild their sense of security. Additionally, professional interventions combined with your unwavering support create the strongest foundation for recovery.
Each child’s healing path unfolds uniquely—what works for one may not work for another. Therefore, remain flexible while maintaining the consistent presence your child needs. Community resources can strengthen your support network during this journey; organizations like Support A Child’s Light offer valuable assistance for families navigating trauma recovery together.
Trauma may be part of your child’s story, but it need not define their future. Children who receive appropriate support after traumatic experiences often develop exceptional resilience, empathy, and emotional intelligence. Consequently, your commitment to understanding trauma’s effects and supporting recovery represents an invaluable gift that will benefit your child throughout their lifetime.
The road to healing may sometimes feel challenging, but hope remains your most powerful ally. Celebrate small victories, maintain connections, and trust in your child’s innate capacity for growth. Indeed, with your support, your child can move beyond trauma toward a future defined not by past wounds but by strength, resilience, and possibility.
FAQs
Q1. What are some common signs of childhood trauma? Common signs include changes in mood or personality, social withdrawal, aggressive behavior, sleep disturbances, difficulty concentrating, and physical complaints like headaches or stomachaches. Children may also exhibit regression in developmental milestones or heightened alertness to perceived dangers.
Q2. How can parents talk to their children about traumatic events? Use age-appropriate language, be honest, and encourage open communication. Start by asking what they already know, correct misconceptions, and provide accurate information. Reassure them of their safety, validate their emotions, and be patient with their questions. Avoid euphemisms and be prepared to have multiple conversations over time.
Q3. What role does a child’s home environment play in trauma recovery? A supportive home environment is crucial for trauma recovery. Create a physically and emotionally safe space by reducing potential triggers, maintaining consistent routines, and offering calming activities. Encourage autonomy by giving age-appropriate choices and involve the child in creating their own safe spaces within the home.
Q4. How can schools support children who have experienced trauma? Schools can support trauma-affected children by implementing trauma-informed practices, providing staff training, creating safe spaces, and using positive behavioral supports. Collaboration between parents, teachers, and counselors is essential. Schools can also help connect families with local mental health resources and maintain normal routines to provide stability.
Q5. What are some effective treatments for childhood trauma? Evidence-based treatments include Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Dialectical Behavior Therapy for Children (DBT-C). These therapies focus on processing traumatic memories, developing coping strategies, and improving emotional regulation. Family involvement in treatment often leads to better outcomes.